Monitoring Treatment of Children
Scott A. Rivkees, M.D.
Associate Professor
Director, Yale Child Health Research Center
Section of Pediatric Endocrinology
Yale Department of Pediatrics
Overview
Monitoring treatment in congenital adrenal hyperplasia (CAH) is as important as the treatment itself. Yet, monitoring approaches vary from institution to institution and from doctor to doctor. The recent CAH consensus statement addressed many important aspects related to the care and treatment of CAH. Yet, no specific recommendations were given related to desired hormone levels. Many articles and textbook chapters about CAH also emphasize the importance of monitoring, yet few provide specific details. Not surprisingly, parents and individuals with CAH find it difficult to obtain clear information about acceptable hormone levels and appropriate testing regimens in CAH.
Although it may seem that monitoring and testing in CAH is confusing, there are several approaches that can be used to adequately assess hormone production. It is also very important to emphasize that monitoring changes in physical growth and maturation is as important, if not more important, as the laboratory testing in CAH.
Growth & Bone Density
Monitoring growth and maturation in CAH
Growth and weight: The rate of growth provides very important clues about treatment in CAH. In general, with proper treatment the child with CAH should grow along the same percentile for height, which reflects the height of the parents.
Between two years of age and puberty, the average child grows about 2-1/2 inches per year and gains 2-3 pounds for every inch of height gain. During infancy and puberty, rates of growth are even faster than during childhood. In general, a child will usually grow along the same percentile on growth charts from infancy though adolescence. Thus, height and weight need to be both monitored and plotted on standard growth charts to assess growth in CAH.
Looking at growth charts and following changes in height and weight, one can detect signs of over- and undertreatment. If glucocorticoid (hydrocortisone, prednisone, dexamethasone) doses are too high, growth will slow and weight will increase. It takes about 3-6 months to appreciate changes in growth rates (changes in height). Changes in weight, though, can be seen much sooner. Increases in weight, above and beyond that which are normally expected (more than 3 lbs per inch of growth; more than 7 lbs per year), can be a sign of overtreatment. Thus, it is very useful for families to monitor weight at home. For example, if the weight increases by more than one pound over 2-4 weeks after a dose change, it may be a sign that the dose is too high.
Whereas slowing of growth can represent signs of overtreatment, increased growth can reflect undertreatment. With undertreatment, there is increased androgen production, which can stimulate growth. Undertreated children may therefore climb to higher height percentiles on growth charts.
The importance of regular follow-up
To assess physical changes in CAH and be able to respond to signs of over- or undertreatment in a timely manner, many practitioners will see individuals with CAH every 3-4 months. Because signs of over-treatment (facial roundness) can be subtle, it is preferable to see the same practitioner at each visit.
There are physical signs that clinicians can see that suggest either over- or undertreatment. With overtreatment, the face can become round. With significant overtreatment, striae (purple “stretch-marks”) can occur. Features of undertreatment include dark or “dirty”-looking knuckles caused by excessive ACTH secretion. Stomach pain and being excessively tired are also symptoms of undertreatment.
The blood pressure can provide clues about mineralocorticoid (Florinef, fludrocortisone) treatment. If the blood pressure is elevated, this may indicate that the mineralocorticoid dose or salt supplementation is too high and should be reduced. Yet, if the dose is normal or too low, the blood pressure is normal.
Signs of pubertal development are also monitored. In girls, one of the earliest signs of puberty is breast development. In boys, enlargement of the size of the testes is the earliest signs that puberty has started. If puberty begins less than seven years of age in girls and less than nine years of age in boys, it is said to be early or “precocious”. Because the adrenal hormones can affect the pituitary gland, precocious puberty is seen in CAH and warrants attention.
The Usefulness of Bone Ages
One of the best tools for monitoring changes in physical maturation is the “bone age”. The growth centers, which can be easily visualized with an x-ray of the hand, provide a wonderful marker of long-term androgen secretion. As children get older, the shape of the growth centers change and have characteristic appearances at each age. By comparing the size and shapes of the growth centers in the child’s hand to those found in a book of standards, a “bone age” can be determined. Because there is variability from practitioner to practitioner in bone age interpretation, it is useful to have bone ages interpreted by the same individual. Also, some pediatric endocrinologists may be more experienced in interpreting bone ages than general radiologists.
When there is excessive androgen secretion, the skeleton matures at a more rapid pace than usual. This will result in an advanced bone age. Thus, an undertreated child at 6 years of age may have a bone age of 9 years of age. Yet, if the bone age is within a year or so of the actual age, this suggests that treatment has been fine.
The bone age also reflects hormone secretion over the preceding 6-12 months. Changes in the bone age may lag behind recent periods of excess androgen secretion. Many practitioners therefore obtain bone ages every 6 to 12 months.
LABORATORY TESTING
Monitoring of Hormone Levels in CAH
The levels of adrenal hormones in the blood vary over the 24-hour day. Cortisol and androgen production is highest in the morning and lowest in the afternoon and evening. Hormone levels are also affected by medications. Following a dose of glucocorticoids, androgen levels will fall. Yet, as the medication wears off, hormone levels may rise excessively. Care must be taken to consider the time of day and the timing of doses when interpreting hormone levels.
There are several different approaches that can be used to assess adrenal hormone production. Urine testing is a “gold standard” and can be used to measure hormone production throughout the day. Blood testing provides important information about hormone production and is preferred by many clinicians due to convenience. Testing of hormone levels several times a day using filter paper specimens has also been shown to be an effective monitoring tool, but is not widely available.
Urine Testing
A single blood test measures androgen levels at one time of day. In comparison, a 24-hour urine collection reflects androgen secretion over the 24-hour day and is therefore recognized as the “gold standard” in assessing hormone production.
To assess adrenal hormone production one measures 17 ketosteroids (17KS) and pregnanetriol in the urine. The 17 KS are breakdown products (metabolic products) of androstenedione and testosterone. Pregnanetriol is the breakdown product of 17-hydroxyprogesterone (17 OHP).
Creatinine is also measured in urine samples. Creatinine is a breakdown product of muscle and is continuously released into the urine. It is produced at a rate of about 10-15 mg/kg (4-6 mg/lb) per day. Measuring the amount of creatinine in the sample indicates if the 24-hour collection is complete or incomplete.
Urine collections are saved in containers provided by hospital or commercial laboratories. They can be conveniently collected on a weekend day and avoid or reduce the need for blood-sticks. Collections are performed by having the child urinate into the toilet on the morning that the collection starts. The urine is then collected over the entire day, and the urine from the first void the following morning is also collected. The container is kept in a cool place until it is brought to the laboratory.
The elimination of 17 KS and pregnanetriol in the urine increases with age. The values obtained in a 24-hour collection can be compared to normal rates of excretion. 17 KS levels provide the best marker of androgen production. Even in situations in which there is adequate treatment, pregnanetriol levels can be elevated. Thus, when 17 KS and pregnanetriol levels do not agree, more emphasis should be placed on the 17 KS value.
Blood Testing
Assessing control from a single blood test is very commonly used due to its convenience. However, a single test may not always reflect if there is adequate control of adrenal gland activity. One also needs to consider the time of day and the timing of doses in interpreting blood levels. Some hormone levels are also better than others in assessing treatment.
A number of hormones that reflect adrenal gland activity can be measured in the blood. These factors include ACTH, 17 hydroxyprogesterone (17 OHP), androstenedione, and testosterone. Electrolytes and renin are used to assess mineralocorticoid replacement.
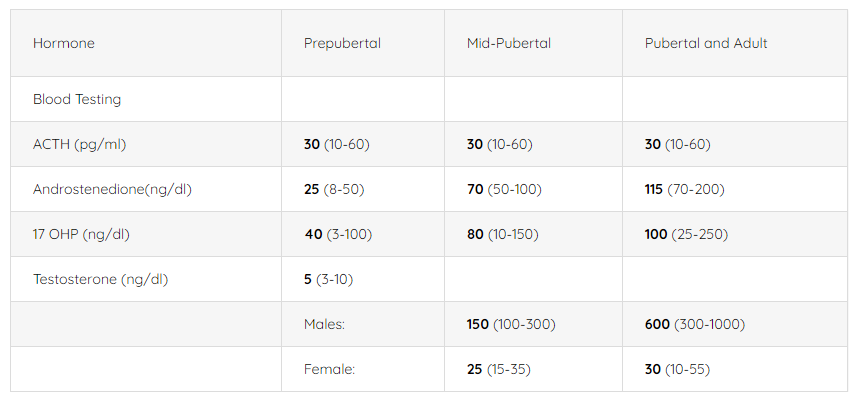
Of these different hormones, androstenedione and testosterone most closely match 24-hour 17 KS production and reflect adrenal androgen production. These hormones are especially useful in prepubertal children and females. Because testosterone levels rise in puberty in males, testosterone levels are not as useful in adolescent or adult males. In comparison with androstenedione and testosterone, 17 OHP levels can fluctuate widely and may be elevated even when there is good control. The pituitary hormone ACTH has been shown to provide a nice measure of control and is elevated 75% of the time when there is undertreatment.
For children without CAH and who are not in puberty, average levels of androstenedione are 25 ng/dl, average levels of testosterone levels are 5 ng/dl, and average 17OHP levels are 50 ng/dl. During puberty, levels of these hormones rise. It is possible to achieve normal levels of these hormones in children with CAH. Yet, treating CAH to “normalize” all hormone levels, especially 17 OHP levels, can result in growth suppression and weight gain. Thus, many clinicians aim for androstenedione and testosterone levels that are normal or modestly (about 25%) above normal. Because 17 OHP levels can fluctuate widely and be elevated when there is adequate treatment, some clinicians will accept mid-day 17 OHP levels of 500-1000 ng/dl; others will aim for lower levels.
Morning levels of 17 OHP, androstenedione, and testosterone are much higher than mid-day levels, especially when there is undertreatment. This occurrence reflects the general observation that adrenal glands become more active in the early morning hours and at a time when the medication from the day before is wearing off. It can therefore be very useful to obtain morning hormone levels.
It has been recently shown that when there is good control of adrenal gland activity, 17 OHP levels are less than less than 600 ng/dl in the morning before medication is given and less than 200 ng/dl during the day. In undertreated individuals, 17 OHP levels average 10,000 ng/dl in the morning before the dose, and 5000 ng/dl during the day.
To measure if the child is getting enough salt and/or fludrocortisone, renin and electrolyte levels are measured. An elevated renin levels indicates a need for more salt and/or fludrocortisone. A suppressed renin suggests that the dose of salt and/or fludrocortisone is too high.
Filter Paper Specimens
Whereas a single blood test during the day can provide important insights into CAH control, they can sometimes be misleading. If a sample is obtained in an undertreated child a few hours after a dose of hydrocortisone has been given, levels of 17OHP can decrease. As the medication wears off, 17 OHP levels can increase dramatically.
One can overcome potential pitfalls of obtaining once daily samples by obtaining filter-paper specimens over the course of the day. Children with diabetes check their blood sugar by finger stick 3-4 times a day to be able to properly dose insulin levels. Similarly, one can measure 17 OHP levels on filter paper specimens taken at different times of day. Thus, one can identify times of day when levels are high and others when levels are low and adjust doses accordingly. Filter paper 17OHP levels can be measured by state laboratories that perform newborn screening for CAH using filter-paper specimens.
Normal Hormone Levels (not CAH):
Urine testing
17 Ketosteroids (mg/24 hr) 1.5 (0.2- 3) Males 5 (3-10) 15 (10-25)
Female 3.5 (2.5-8) 10 (6-14)
Pregnanetriol (mg/24 hr) 0.5 1.0 2.0
-In CAH, levels of androstenedione, testosterone and 17 ketosteroids that are normal or modestly (about 25%) above normal are acceptable. Because blood 17 OHP levels can vary widely in CAH, higher 17 OHP levels are acceptable, but are usually less than 1000 ng/dl with adequate treatment.
-To convert ng/dl units to pmol/L, multiply androstenedione levels by 34, 17 OHP by 30, testosterone by 34.
Conclusions
The proper monitoring the child with CAH is essential for optimizing treatment and ensuring normal development. Following height and weight is extremely important in the monitoring process, and frequent follow-up is recommended. Bone ages are useful, as they reflect long-term androgen secretion. The measurement of 17 KS in the urine, or androstenedione or testosterone in the blood provides nice measures of adrenal androgen production. Although published specific recommendations for the acceptable hormone levels in CAH are few, many clinicians will aim for levels of androstenedione, testosterone and 17 KS that are normal or modestly (about 25%) above normal. Because blood 17 OHP levels can vary widely in CAH, higher than normal 17 OHP levels are acceptable, but are usually less than 1000 ng/dl with adequate treatment. Because there are different ways to assess if treatment is effective, it is important that you know and understand your physician’s approach in monitoring CAH.


CONTACT
2414 Morris Avenue, Ste 110
Union, NJ 07083
Phone: (908) 364-0272
Toll Free: (866) 227-3737
Fax: (908) 686-2019
contact@caresfoundation.org




